|
|
|
| Gingival Depigmentation: A Comparison Between Three Techniques |
Preeti Upadhyay 1 , Ashish Verma 2 , Dimple Grover 3 , Swati Sanghi 4
1 Reader , Dept. of Periodontology - Manav Rachna Dental college
2 Associate Professor, Dept. Of Periodontics - Manav Rachna Dental College, Faridabad
3 Associate Professor, Dept. of Oral & Maxillofacial Surgery - Manav Rachna Dental College
4 Associate Professor , Dept. of Conservative Dentistry - Manav Rachna Dental College.
|
| Address For Correspondence |
Dr. Preeti Upadhyay
J- 115, Saket New Delhi.
EmailID : preeti.mynk@gmail.com
MobileNo : 09910012441 |
| Abstract |
| Gingival hyperpigmentation due to melanin deposition is seen as a genetic trait in most of the population irrespective of age and gender hence it is termed physiologic or racial gingival pigmentation. Many people are unhappy with their unaesthetic gingival appearance and find the discoloration to be very unappealing and detracting from their smile and speech. Usually, this condition is a cosmetic issue and not necessarily a sign of a dental health problem. The problem can be treated by number of surgical techniques selection of which might be based on clinical experiences and individual preferences, of the operator. |
|
| Keywords |
| Depigmentation, scalpel technique, bur abrasion, electro surgery. |
|
| Full Text |
Introduction:
It is not uncommon to find pigmented lesions in the oral cavity. Such lesions represent a variety of clinical entities, ranging from physiologic changes (e.g., racial pigmentation) to manifestations of systemic illnesses (e.g., Addison’s disease) and malignant neoplasms (e.g., melanoma and Kaposi’s sarcoma). Oral pigmentation may be exogenous or endogenous in origin. Exogenous pigmentation is commonly due to foreign-body implantation in the oral mucosa. Endogenous pigments include melanin, hemoglobin, hemosiderin and carotene. Melanin, a brown pigment, is the most common natural pigment contributing to endogenous pigmentation of gingiva. Melanin pigmentation is the result of melanin granules produced by melanoblasts intertwined between epithelial cells at the basal layer of gingival epithelium.[1]
In this day and age people have become increasingly aware of their physical appearance. Correspondingly aesthetic treatment modalities have become more and more popular. There has been a rise in the number of patients who are dissatisfied with the pigmentation of their gingiva, finding it unappealing and detracting from their smile. They find it a cause of embarrassment and seek different forms of treatment in order to attain what they consider a ‘perfect’ smile.
Gingival depigmentation is a periodontal surgical procedure in which the gingival hyperpigmention is eliminated or reduced by different techniques[2].
Selection of technique should be based on clinical experiences and individual preferences.
This case report presents a comparison between three depigmentation procedures.
Case Description:
A 23 year old male patient reported to the OPD of Periodontology MRDC, with the chief complaint of “black” colored unaesthetic gums whichinterfered with his smile. On intraoral examination, generalized blackish pigmentation of gingiva was observed from right premolar to left premolar on both maxillary and mandibular arches. (Figure 1). The patient’s history revealed that the blackish discoloration of gingiva was present since birth suggestive of physiologic melanin pigmentation. His medical history was non-contributory. Considering the patient’s concern, a split mouth surgical gingival de-epithelization procedure was decided for both the arches.
 | Table 1 - Methods To Remove The Pigment Layer
 |
 | Figure- 01 Unaesthetic Blotchy Black Gingiva.
 |
Before depigmentation procedure complete scaling and polishing were done and patient was given oral hygiene instructions. The entire procedure was explained to the patient and written consent was obtained and he was also informed about the recurrence rate of repigmentation. Complete medical and family history was recorded and blood investigations were carried out to rule out any contraindication(s) for surgery.
Visit 1:
Scalpel Technique:
A scalpel surgery was planned to perform the depigmentation on right side in maxillary arch. Local anesthesia was infiltrated in the maxillary anterior region from right premolar to left premolar (Lignocaine with adrenaline in the ratio 1:100000 by weight). A partial split thickness flap was raised on right side using a Bard Parker handle with a No.15 blade, maintaining the normal architecture of gingiva. Bleeding was controlled using pressure pack with sterile gauze. (Figure 2 depigmentation with scalpel and blade).
 | Figure- 02 Depigmentation With Scalpel And Blade.
 |
Bur Abrasion Technique:
The bur abrasion technique was used on left side for deepithelization of heavily pigmented gingiva using high speed rotary instrument. After adequate local anesthesia, large straight bur was used along with copious saline irrigation. Pressure was minimal with feather light brushing strokes without holding bur in one place to avoid pitting of the gingival surface or to remove too much tissue. Care was taken to remove all the remnants of melanin pigment as thoroughly as possible and a scraping procedure using the scalpel blade was used for the purpose, but at one point the tissue was fenestrated. (Figure 3 & Figure 4 ).
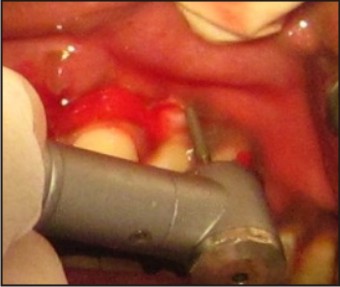 | Figure- 03 Depigmentation With Bur Abrasion
 |
 | Figure- 04 Post-operative.
 |
The surgical area was covered with periodontal dressing. Post-surgical antibiotics (Amoxicillin 500mg, thrice daily for five days) and analgesics (Ibuprofen with Paracetemol, thrice daily for three days) were prescribed. The patient was advised to use Chlorhexidine mouthwash 12 hourly for one week.
After 2 weeks, the pack was removed and the surgical area was examined. The healing was uneventful without any post-surgical complications. The gingiva appeared reddish pink and firm giving a normal appearance. The patient was happy and satisfied with the outcome of the procedure.
Visit 2:
For mandibular arch, a combination of scalpel de-epithelization, and electrosurgery was planned.
Electrosurgery:
Electrosurgery was performed for mandibular right side using loop electrode and ball electrode. Minimal bleeding with a clean field increased the efficacy of the procedure. Light brushing strokes were used and the tip was kept moving all the time. Prolonged or repeated application of electrode to the tissues was avoided as it induces heat accumulation; enough care was taken to avoid contact with the periosteum and vital teeth. Patient was more comfortable with this procedure, as he kept saying during the procedure. (Figure - 05, 06, 07, 08).
 | Figure- 05 Depigmentation With Electro Cautery, Bloodless Surgical Site Can Be Appreciated.
 |
 | Figure- 06 Depigmentation With Scalpel And Blade.
 |
 | Figure- 07 Post-operative.
 |
 | Figure- 08 Post-operative 6 Months, Healthy Firm Pink Gingiva Can Be Appreciated.
 |
Scalpel Technique:
Deepithelization on mandibular left side was performed with scalpel technique. Post operative instructions were given to the patient. (Figure 6, Figure 7).
Patient was recalled after 15days for checkup.Healing was satisfactory.
The gingiva was healthy firm pink even at the end of 6 months, repigmentation has not started (Figure 8).
Discussion
The color of the gingiva is determined by several factors, namely number and size of the blood vessels, epithelial thickness, quantity of keratinization and pigments within the gingival epithelium[13]. Hyperpigmentation of the gingiva is caused by excessive melanin deposition by the melanocytes mainly located in the basal and suprabasal cell layers of the epithelium.[14] Melanin pigmentation may be seen across all races and at any age, and has no gender predilection.[15] A positive correlation between gingival pigmentation and the degree of pigmentation in the skin, seems, however, evident.[16] Demand for treatment is usually made for esthetic reasons.To treat depigmentation and to enhance esthetics, numerous techniques have been employed from time to time. Selection of a technique should be based on clinical experience and individual preferences. This case report compares three different techniques commonly used to treat depigmentation and compiles the advantages and disadvantages of each technique.
Scalpel Technique:
It is the most simple and effective method of depigmentation which does not require any sophisticated instruments.The procedure essentially involves surgical removal of the gingival epithelium along with a layer of the underlying connective tissue under adequate local anesthesia and allowing the denuded connective tissue to heal by secondary intention. The new epithelium that forms is devoid of pigmentation. [17], [18]
However, it results in unpleasant hemorrhage during or after surgery. Hence, it is necessary to cover the lamina propria with periodontal dressing for 7-10 days.[4] It also has chances of infection or recurrence. Results reported are excellent. [19]
Bur Abrasion:
It is a simple and easy method that does not require any sophisticated equipment. Healing occurs by secondary intention thus pre- and post-surgical care is similar to that of the scalpel technique. However, extra care should be taken to control the speed and pressure of the handpiece bur so as not to cause unwanted abrasion, fenestration or pitting of the tissue. Minimum pressure with feather light brushing strokes and copious saline irrigation should be used without holding the bur in one place to achieve good results. [20]
ElectroSurgery:
Electrosurgery has advantages of minimal bleeding and a cleaner work field. According to Oringer's "Exploding cell theory,"[21] it is predicted that electrical energy leads to the molecular disintegration of melanin cells of the operated and surrounding sites. Thus, electrosurgery has a strong influence in retarding migration of melanin cells. However, electrosurgery requires more expertise than the techniques mentioned. Prolonged or repeated application of current to the tissues induces heat accumulation and undesired tissue destruction.[4] Contact of current with the periosteum and vital teeth should be avoided.[22]
Though the initial result of the depigmentation surgery is highly encouraging, repigmentation is a common problem. The exact mechanism of repigmentation is not known. Different studies shows variation in the timing for early repigmentation.[22] To return to full clinical baseline repigmentation it takes about 1.5 to 3 years.[13] This variation may be due to the techniques performed or due to the patient’s race. Thus, gingival depigmentation procedure, if performed primarily for cosmetic reason, will not be of permanent value. However, even if gingival repigmentation occurs in the patient, depigmentation can be repeated in the same region.
In the present case report three different depigmentation surgical procedures were performed in same patient. While performing the surgical procedure, electrosurgery appeared to be the most convenient technique, as it was quick and without hemorrhage, followed by scalpel blade because in this procedure we were able to control the depth of incision. Although depigmentation with bur abrasion was quick but hemorrhage during surgical procedure was more and it was difficult to control the depth, in our case fenestration occurred in the area with thin gingiva in the left maxillary canine region. Post operatively patient was most comfortable with electrosurgery.
Conclusion:
This case report describes simple and effective surgical procedures for the treatment of gingival melanin hyperpigmentation resulting in improved esthetics and cosmetic appearance, thereby increasing the self confidence of the patient. The above mentioned procedures can be performed by general dental practitioners to improve dark pigmented gingival appearance, but patient should be informed of high chances of repigmentation.
References:
1. Eisen D. Disorders of pigmentation in the oral cavity. Clin Dermatol 2000; 18(5):579–87.
2. Roshna T, Nandakumar K. Anterior Esthetic Gingival Depigmentation and Crown Lengthening: Report of a Case. J Contemp Dent Pract 2005; (6)3:139-147.
3. Putter OH, Ouellet D, Putter A, Vilaboa D,Vilaboa B, Fernandez M. A non-traumatic technique for removing melanotic pigmentation lesions from the gingiva: Gingival abrasion. Dent Today 1994;13(10): 58-60.
4. Gnanasekhar JD, Al-Duwairi YS. Electrosurgery in dentistry. Quintessence Int 1998; 29(10):649-654.
5. Tal H, Landsberg J, Kozlovsky A. Cryosurgical depigmentation of the gingiva. A case report. J Clin Periodontol 1987; 14(10):614-617.
6. Yeh CJ. Cryosurgical treatment of melanin-pigmented gingiva. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86(6):660-663.
7. Treatment of gingival hyperpigmentation for esthetic purposes by Nd:YAG laser: Report of 4 cases. J Periodontol 2000;71(2):315-321.
8. Yousuf A, Hossain M, Nakamura Y, Yamada Y, Kinoshita J, Matsumoto K. Removal of gingival melanin pigmentation with the semiconductor diode laser: A case report. J Clin Laser Med Surg 2000;18(5):263-266.
9. Nakamura Y, Hossain M, Hirayama K, Matsumoto K. A clinical study of the removal of gingival melanin pigmentation with the CO2 laser. Lasers Surg Med 1999; 25(2):140-147.
10. Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int. 1996; 27(8):555-558.
11. Hirschfeld I and Hirschfeld L. Oral pigmentation and method of removing it. Oral Surg Oral Med Oral Path. 195;4:1012.
12. Fowler EB, Breault LG, Galvin BG. Enhancing physiologic pigmentation utilizing a free gingival graft. Pract Periodontics Aesthet Dent. 2000;12(2): 193-196.
13. Begamaschi O, Kon S, Doine AI, Ruben MP. Melanin repigmentation after gingivectomy: A five year clinical and transmission Electron Microscopic Study in Humans. Int J Periodontol & Restorative Dent.1993; 13(1):85-92.
14. Cicek Y, Ertas U. The normal and pathological pigmentation of oral mucous membrane: a review. J Contemp Dent Pract. 2003:15; 4(3):76-86.
15. Dummett, C.O: Oral pigmentation. First symposium of oral pigmentation. J Periodontol. 1960;31:356.
16. Dummett CO, Sakumura JS, Barens G. The relationship of facial skin complexion to oral mucosa pigmentation and tooth color. J Prosthet Dent 1980;43(4):392- 396.
17. Almas K, Sadig W. Surgical treatment of melanin pigmented gingiva: An esthetic approach. Indian J Dent Res. 2002;13:70–3.
18. Kathariya R, Pradeep AR. Split mouth de-epithelization techniques for gingival depigmentation: A case series and review of literature. J Ind Soc Periodontol. 2011;15(2):161-168.
19. Kanakamedala AK, Geetha A, Ramakrishna T, Emadi P. Management of gingival hyperpigmentation by the surgical scalpel technique: Report of three cases. J Clin Diag Res.2010;4:2341–6.
20. Deepak P, Sunil S, Mishra R, Sheshadri Treatment of gingival pigmentation: A case series. Indian J Dent Res. 2005;16:171–6.
21. Gage AA, Baust J. Mechanisms of tissue injury in cryosurgery. Cryobiology. 1998; 37:171–86.
22. Perlmutter S, Tal H. Repigmentation of the gingiva following surgical injury. J Periodontol. 1986;57(1):48-50. |
|
|
|
|
|
|